By December, Gilead expects to produce enough of the drug to treat 2 million patients, and is exploring an inhaled form of it for outpatients.
The United States reached a milestone, of sorts, when last week the Food and Drug Administration approved the first treatment for COVID-19.
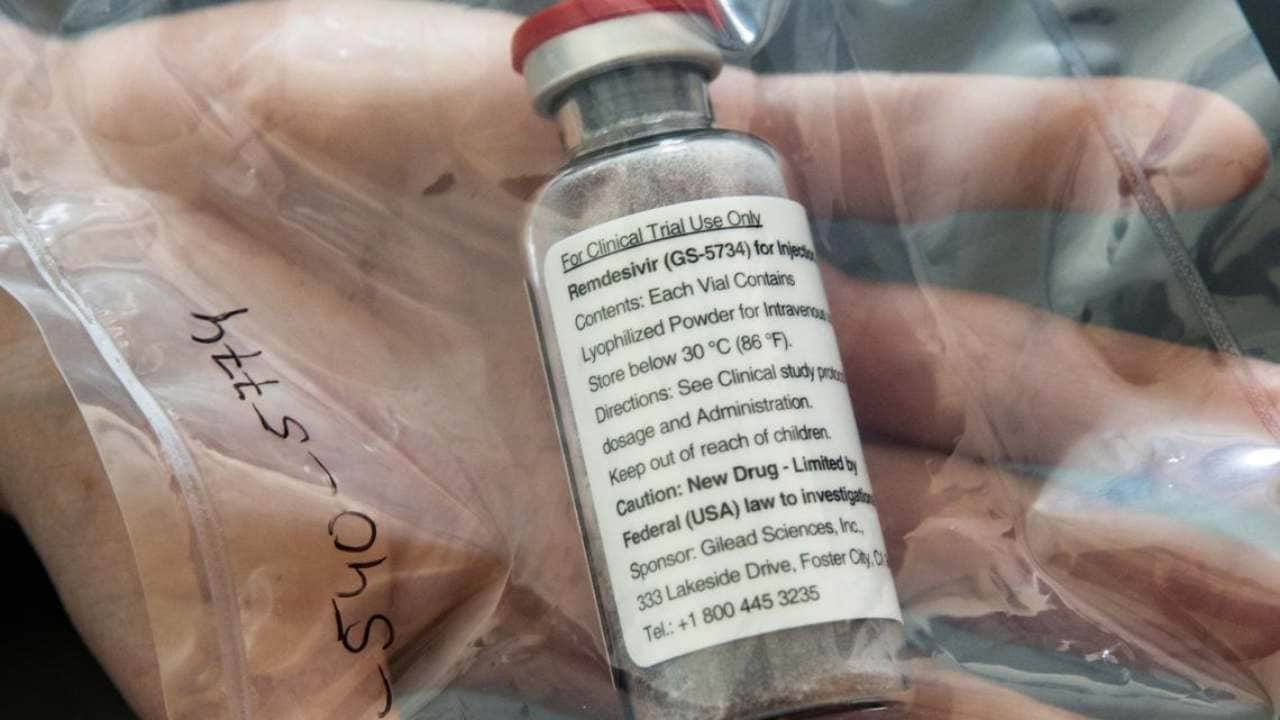
The drug is called Veklury, although most people know it by its scientific name, remdesivir.
On Wednesday, its manufacturer, Gilead Sciences, said that remdesivir, which has been authorized for emergency use since the spring, had brought in $873 million in revenues so far this year and that it was the company’s second-best-selling drug in the third quarter, behind its HIV drug, Biktarvy.
But the FDA’s decision to grant the drug full approval — which means the company can begin broadly marketing it to doctors and patients — has puzzled several outside experts, who say that it may not deserve the agency’s stamp of approval because it is, at best, a mediocre treatment for COVID-19, the disease caused by the coronavirus. And they have questioned whether Gilead deserves to pocket potential billions from the drug when the federal government has played a significant role in its development.
“This is a troubling approval,” said Dr. Peter B. Bach, director of the Center for Health Policy and Outcomes at Memorial Sloan Kettering Cancer Center. “This is an extremely weak set of trials to support an approval for an antiviral.”
Remdesivir was seen as one of brightest hopes in the dark days of March and April, when doctors had few tools to treat a new disease and families rushed to gain access to the drug in a desperate gambit to save their dying relatives.
More than six months later, enthusiasm has fizzled. One large, government-run trial showed that the drug shortens patients’ recovery times, but the two other studies the FDA used to justify its approval — sponsored by Gilead — did not compare the treatments with a placebo, the gold standard for evaluating a drug. No studies have shown that it significantly lowers death rates.
And just days before the FDA granted approval, a large study sponsored by the World Health Organization found that remdesivir provided no benefit to hospitalized patients.
“I think most people think that because a drug is FDA approved, that means it must work,” said Dr. Aaron S. Kesselheim, a professor of medicine at Harvard Medical School who studies the drug industry. He and other researchers recently found that less than one-third of new drugs approved by the FDA and its European counterpart over the past decade were rated as having a “high therapeutic value” by outside experts.
“I think it’s important to recognize that FDA approval doesn’t guarantee a certain level of benefit — all it says is that there is some benefit,” he said.
On a call with investors Wednesday, Gilead’s chief executive, Daniel O’Day, said remdesivir had a role to play, along with vaccines and other treatments.
“There’s a lot we don’t know about the pandemic, of course, but I think what we do know is that in order to get us all back to normal, this is going to take a variety of approaches,” he said. “We’re proud to be at the front end of this with a very potent antiviral.”
Remdesivir was originally developed as a treatment for Ebola and hepatitis C and is thought to interfere with the reproduction of viruses by jamming itself into new viral genes.
Because it had previously shown promise in animal studies of other coronaviruses, it was almost immediately seen as a possible answer for COVID-19. Gilead rushed emergency doses to China and began ramping up manufacturing.
The drug was initially used on the very sick but has since been found to work better earlier in the course of the disease. It is routinely given as a five-day treatment to people who are hospitalized for COVID-19, including to President Donald Trump when he was infected earlier this month.
Gilead has come under criticism for its efforts to profit from the drug. In March, when there were still fewer than 200,000 cases of COVID-19, the company applied to the FDA to label remdesivir as an orphan drug, a designation that provides tax and other incentives to companies developing products for rare diseases. After a public outcry, it asked the FDA to rescind its application.
Gilead has gotten mixed reviews from outside experts over the price it has set, at $3,120 for a course of treatment for private insurers and $2,340 for government entities.
One outside group that evaluates drug prices, the Institute for Clinical and Economic Review, said Gilead had made a “responsible pricing decision” that was in line with its own determination that $2,800 would be a fair price. However, that praise came with a significant caveat — the price would be fair only if remdesivir ultimately showed that it significantly lowered death rates, a benefit that has not been proven.
Others say the company’s profits are unfair, given how much support it has gotten from the government. Public Citizen, a consumer group, has estimated that the federal government has invested $70 million in remdesivir, and it sponsored the major trial that led to FDA approval — and the only major study that compared it with a placebo.
“Remdesivir should be in the public domain,” said Peter Maybarduk, director of the global access to medicines program at Public Citizen. “Gilead will have remade its modest investment many times over.”
In August, attorneys general from 34 states wrote to federal health officials asking them to exercise so-called march-in rights to alleviate shortages of the drug (which have since been resolved). And in September, 11 state treasurers wrote to the company, asking it to price the drug “more affordably.”
In a statement, Gilead said that its own investments in the drug this year “will exceed $1 billion, primarily due to early investments in the rapid scale up of manufacturing, and we expect to invest significantly more in 2021 as we make additional investments in development and manufacturing around the world.”
The company said that by December, it expected to have produced enough drug to treat 2 million patients and that it was studying an inhaled form of the drug that could expand its use to outpatients.
Last week, Gilead came under new criticism because when remdesivir was approved, the company was awarded a priority review voucher, an incentive that allows it to get expedited review from the agency for a future product or to sell that right to another company. The vouchers, which can sell for about $100 million on the open market, are awarded to companies that develop products — such as ones that address a public health threat like a pandemic — that might not otherwise be profitable.
But remdesivir is already proving to be a significant moneymaker for Gilead.
“The idea behind the priority review vouchers program is that there’s relatively little financial incentives for companies to make drugs for some of these conditions,” said Rachel Sachs, an associate professor of law at Washington University in St. Louis who studies drug policy. “If we think that this drug will be a blockbuster, then the reasons why we created the program would seem to apply with much less force here.”
The FDA’s approval was surprising to some because it came just days after the release of results from the Solidarity trial, a large, global study of more than 11,000 people that found that remdesivir did not reduce deaths.
Both the FDA and Gilead have noted, however, that the Solidarity trial had shortcomings, including that it was not compared with a placebo, as the trial sponsored by the National Institutes of Health was.
Now that Veklury is FDA-approved, Gilead can begin marketing it, including to doctors and hospitals that might be reluctant to use the treatment.
Gilead said it did not plan to run television advertising for Veklury but would deploy a “field team of medical and sales professionals to educate health care professionals across the country.”
It said it also had plans “to develop some direct-to-consumer materials on Veklury, focused on providing information and education for patients and their families.”
Veklury’s future sales are uncertain. On the call with investors, executives said that predicting revenues in the middle of a pandemic is difficult. Around 40% to 50% of hospitalized COVID-19 patients receive the drug — fewer than some industry analysts had expected. But the drug is profitable so far. One Wall Street analyst, Geoffrey Porges of SVB Leerink, said Thursday that the company’s gross margin on sales to the government — the amount it pockets after the cost to produce it — appeared to be about 90%.
In the call with investors, O’Day said that he expected Veklury to ultimately provide a “very good return” on the company’s investment. “We do feel very strongly that Veklury will contribute to our overall sales, being an important source of cash for our business,” he said.
Bach, of Memorial Sloan Kettering, said that as doctors’ knowledge of COVID-19 had evolved, the significance of remdesivir had receded in favor of other options, including dexamethasone, a steroid made by several generic drug companies.
Because the steroid is a cheap, widely available drug whose patent protections have long since expired, there is little incentive for those companies to seek formal approval from the FDA to be able to market the drug for COVID-19.
That gives Gilead a potential marketing advantage, with no other drug company actively competing for sales. But the purpose of an approval is not to grant companies a financial incentive.
“The FDA doesn’t exist to give monetary prizes to drug companies,” Bach said. “The FDA exists to help inform doctors as to what drugs they should give patients in front of them today.”
Katie Thomas. c.2020 The New York Times Company
Post a Comment