The patient in the case report (let’s call him Tom) was 54 and in good health. For two days in May, he felt unwell and was too weak to get out of bed. When his family finally brought him to the hospital, doctors found that he had a fever and signs of a severe infection, or sepsis. He tested positive for SARS-CoV-2, the virus that causes COVID-19 infection. In addition to symptoms of COVID-19, he was also too weak to move his legs.
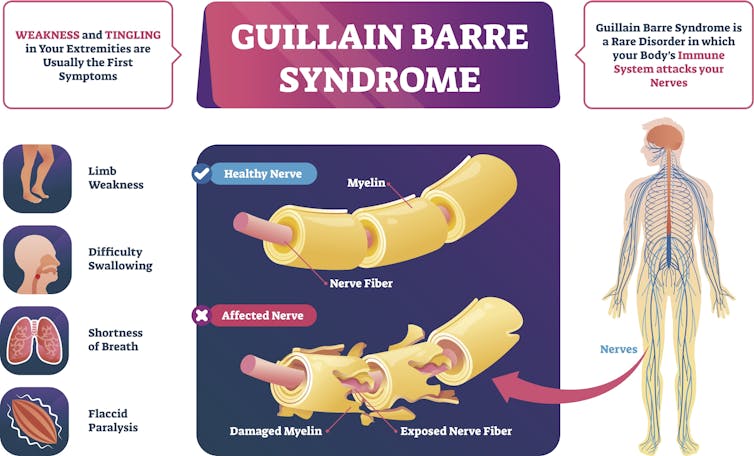
When a neurologist examined him, Tom was diagnosed with Guillain-Barre Syndrome, an autoimmune disease that causes abnormal sensation and weakness due to delays in sending signals through the nerves. Usually reversible, in severe cases it can cause prolonged paralysis involving breathing muscles, require ventilator support and sometimes leave permanent neurological deficits. Early recognition by expert neurologists is key to proper treatment.
We are neurologists specializing in intensive care and leading studies related to neurological complications from COVID-19. Given the occurrence of Guillain-Barre Syndrome in prior pandemics with other corona viruses like SARS and MERS, we are investigating a possible link between Guillain-Barre Syndrome and COVID-19 and tracking published reports to see if there is any link between Guillain-Barre Syndrome and COVID-19.
Some patients may not seek timely medical care for neurological symptoms like prolonged headache, vision loss and new muscle weakness due to fear of getting exposed to virus in the emergency setting. People need to know that medical facilities have taken full precautions to protect patients. Seeking timely medical evaluation for neurological symptoms can help treat many of these diseases.
What is Guillain-Barre Syndrome?
Guillain-Barre syndrome occurs when the body’s own immune system attacks and injures the nerves outside of the spinal cord or brain – the peripheral nervous system. Most commonly, the injury involves the protective sheath, or myelin, that wraps nerves and is essential to nerve function.
Without the myelin sheath, signals that go through a nerve are slowed or lost, which causes the nerve to malfunction.
To diagnose Guillain-Barre Syndrome, neurologists perform a detailed neurological exam. Due to the nerve injury, patients often may have loss of reflexes on examination. Doctors often need to perform a lumbar puncture, otherwise known as spinal tap, to sample spinal fluid and look for signs of inflammation and abnormal antibodies.
Studies have shown that giving patients an infusion of antibodies derived from donated blood or plasma exchange – a process that cleans patients’ blood of harmful antibodies – can speed up recovery. A very small subset of patients may need these therapies long-term.
[Get facts about coronavirus and the latest research. Sign up for The Conversation’s newsletter.]
The majority of Guillain-Barre Syndrome patients improve within a few weeks and eventually can make a full recovery. However, some patients with Guillain-Barre Syndrome have lingering symptoms including weakness and abnormal sensations in arms and/or legs; rarely patients may be bedridden or disabled long-term.
Guillain-Barre Syndrome and pandemics
As the COVID-19 pandemic sweeps across the globe, many neurologic specialists have been on the lookout for potentially serious nervous system complications such as Guillain-Barre Syndrome.
Though Guillain-Barre Syndrome is rare, it is well known to emerge following bacterial infections, such as Campylobacter jejuni, a common cause of food poisoning, and a multitude of viral infections including the flu virus, Zika virus and other coronaviruses.
Studies showed an increase in Guillain-Barre Syndrome cases following the 2009 H1N1 flu pandemic, suggesting a possible connection. The presumed cause for this link is that the body’s own immune response to fight the infection turns on itself and attacks the peripheral nerves. This is called an “autoimmune” condition. When a pandemic affects as many people as our current COVID-19 crisis, even a rare complication can become a significant public health problem. That is especially true for one that causes neurological dysfunction where the recovery takes a long time and may be incomplete.
The first reports of Guillain-Barre Syndrome in COVID-19 pandemic originated from Italy, Spain and China, where the pandemic surged before the U.S. crisis.
Though there is clear clinical suspicion that COVID-19 can lead to Guillain-Barre Syndrome, many important questions remain. What are the chances that someone gets Guillain-Barre Syndrome during or following a COVID-19 infection? Does Guillain-Barre Syndrome happen more often in those who have been infected with COVID-19 compared to other types of infections, such as the flu?
The only way to get answers is through a prospective study where doctors perform systematic surveillance and collect data on a large group of patients. There are ongoing large research consortia hard at work to figure out answers to these questions.
Understanding the association between COVID-19 and Guillain-Barre Syndrome
While large research studies are underway, overall it appears that Guillain-Barre Syndrome is a rare but serious phenomenon possibly linked to COVID-19. Given that more than 10.7 million cases have been reported for COVID-19, there have been 10 reported cases of COVID-19 patients with Guillain-Barre Syndrome so far – only two reported cases in the U.S., five in Italy, two cases in Iran and one from Wuhan, China.
It is certainly possible that there are other cases that have not been reported. The Global Consortium Study of Neurological Dysfunctions in COVID-19 is actively underway to find out how often neurological problems like Guillain-Barre Syndrome is seen in hospitalized COVID-19 patients. Also, just because Guillain-Barre Syndrome occurs in a patient diagnosed with COVID-19, that does not imply that it was caused by the virus; this still may be a coincident occurrence. More research is needed to understand how the two events are related.
Due to the pandemic and infection-containment considerations, diagnostic tests, such as a nerve conduction study that used to be routine for patients with suspected Guillain-Barre Syndrome, are more difficult to do. In both U.S. cases, the initial diagnosis and treatment were all based on clinical examination by a neurological experts rather than any tests. Both patients survived but with significant residual weakness at the time these case reports came out, but that is not uncommon for Guillain-Barre Syndrome patients. The road to recovery may sometimes be long, but many patients can make a full recovery with time.
Though the reported cases of Guillain-Barre Syndrome so far all have severe symptoms, this is not uncommon in a pandemic situation where the less sick patients may stay home and not present for medical care for fear of being exposed to the virus. This, plus the limited COVID-19 testing capability across the U.S., may skew our current detection of Guillain-Barre Syndrome cases toward the sicker patients who have to go to a hospital. In general, the majority of Guillain-Barre Syndrome patients do recover, given enough time. We do not yet know whether this is true for COVID-19-related cases at this stage of the pandemic. We and colleagues around the world are working around the clock to find answers to these critical questions.
Post a Comment