If you know the enemy and know yourself, you need not fear the result of a hundred battles
–Sun Tzu, Chinese general and military strategist, Art of War, 50 BC
From mitigation to suppression strategy: India U-turns and grinds to a halt
Epidemiologists date the first case of pneumonia of unknown origin in Wuhan to mid-November 2019. Over the next month, several more such cases came to Wuhan’s hospitals. By mid-December, Chinese doctors identified a new viral outbreak with its origins in Wuhan’s wet market. But they took another fortnight to report it to the World Health Organization (WHO). By then news of an outbreak of “pneumonia of unknown origin” started circulating on social media. The virus quickly jumped across to Thailand, where the first COVID-19 case outside China was detected on 13 January 2020. A Chinese woman from Wuhan was the carrier (see Box 4: Coronavirus timeline).
The first COVID-19 case in India was detected in Kerala end-January 2020. But like most other countries, India responded sluggishly to the unfolding events. A mild mitigation strategy was put into place only in March. On 12 March, Lav Agarwal, the Ministry of Health and Family Welfare spokesperson stated, “We have only limited local transmission. If we all take the required precautions which are warranted, I am sure that as a country we will be able to manage the situation.”
[embedded content]
On 24 March Prime Minister Modi announced a complete lockdown of India from the next day. Everyone was to remain at home for 3 weeks and all commercial activity, except for the supply of essential goods and services, stopped. Overnight India shifted to a severe suppression strategy. India ground to a halt.
[embedded content]
On 8 April Agarwal stated, “We are getting cases of symptomatic and asymptomatic acting as carriers. When we are dealing with an infectious disease, it is an everyday battle, even a single slipup will cost us. Early identification is key.” The rationale for India’s U-turn—the reasons and triggers used for the decision, whether India had shifted from local to community transmission, the transmission dynamics—continue to remain questions to this day.
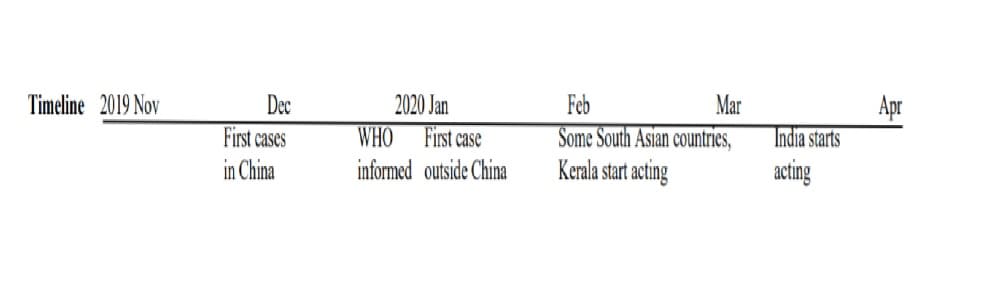
Timeline of the spread of the coronavirus
The Great exodus: Safety principle violated, the virus may strike back
In a trice 44 crore2 unorganized sector workers, including ~1.5 crores were migrants, constituting 94 percent of India’s labour force, became unemployed on 25 March. With no money or food, there was only one thing the migrant workers could do. Return to their villages, a walk of many hundreds of kilometres for most of them.
A few days after the lockdown tens of thousands of migrants went to Delhi’s Anand Vihar Bus Stand to catch the special buses that the UP government had organized for them. Such large gatherings are where disease transmission occurs. Moreover, many of the migrants would carry the virus to their villages, only to carry it back to cities when they returned later. The coronavirus had found new pathways to infect India.

The mass exodus of migrants at Anand Vihar Bus Stand, Delhi
The lockdown flouted a cardinal principle of safety management, “A new safety measure that reduces the risk for a set of persons, should not increase the risk for another set of persons.” If the Tablighi gathering with just a few thousand participants is worrisome, the additional risk of disease spread when thousands of migrants assembled at bus stands in many cities end-March, and again at Bandra Railway Station in Mumbai on 14 April, and in Surat a couple of days before that is alarming.

Migrants walking back to their villages
It appears that no one had advised the Prime Minister that a simple “What if” HAZOP technique should have been used before taking a final call on the first lockdown. It would have predicted the migrants’ mass exodus and suggested a safer action. The returning migrants were put to other risks as well—heart attacks due to exhaustion, hunger, dehydration, and road accidents.
Excesses, inequalities
In his 24 March, speech Prime Minister Modi said “entire India will go under lockdown. This is like a curfew…this is more advanced than Janata Curfew.” In his inimitable style, he announced the lockdown the same way he announced demonetization 3 years ago–suddenly and in a manner that shocked the country. The use of the word ‘curfew’ converted a health crisis into a law and order problem, or that is how law enforcement agencies tend to interpret the word curfew. Since the lockdown began, there have been several reports of police excesses. Surely there are more sensitive ways of making the lockdown announcement and more humane ways of dealing with the public caught in a situation that is not one of their makings.
A few hundred Indians were evacuated by air by the Indian government from China, Italy, and Iran but nobody gave much thought to the lakhs of migrant workers stuck in cities after the lockdown. It was only days after the lockdown that some state governments opened shelters and kitchens for them.
Five thousand migrant workers returning to Bareilly end-March were sprayed with sodium hypochlorite, a bleaching agent that is injuries to eyes and skin. How spraying removes the virus from inside an infected human, and why air evacuees from Wuhan, Iran and Italy were not similarly sprayed remains unexplained.

The police beating a man on a scooter during the lockdown.
India is a water-stressed country and large sections of India’s population barely have one bucket of water per head for their entire daily needs. Where do they have the water to hand wash frequently?
Some West Bengal villages found an innovative but uncompassionate way to do physical distancing. As their homes were small, they encouraged returning migrants to quarantine themselves in trees. Would that be possible in a Mumbai slum where a family of 5-6 persons lives in a 10-20 m2 tenement?
Collateral damage: Mounting humanitarian and economic crises
An economic and a humanitarian crisis are in the making. In time they may become as serious as the COVID-19 health crisis.
With no labour, the rabi harvest that is underway in many states, may suffer. Even if harvesting is completed, without labour farm produce cannot be moved to market yards and from there to consumers. This will have a domino effect. If agricultural produce is not sold, farmers and the agricultural labour lose incomes. And with no money, labour will start going hungry in a few weeks.
The lockdown has come on the heels of an economic slowdown and now has broken the supply chain for production of goods and services. Without replenishment, food grain stocks will deplete in time, raising prices of not just food grains but of other goods and services as well.
When the present lockdown is lifted, the economy will kick not start immediately without labour and working capital. More importantly, demand would have reduced, and cannot be revived immediately, becoming an important factor impeding the ramping up of supply.
The situation in India will be compounded by a global economic slowdown that is in the making. How long recovery will take is moot. If more lockdowns happen, India may stare at the possibility of an increase in hunger and malnutrition, and the spectre of possible food riots.
Testing: Absence of evidence is not evidence of absence
Till 17th March, the test for COVID-19 infection was restricted to symptomatic individuals who had travelled abroad in the last fortnight and symptomatic cases of laboratory-confirmed cases. A symptomatic person who had not been abroad or was not in contact with a confirmed case could not avail of a test. Three days later, more categories of people could be tested–symptomatic health care workers, hospitalized patients with Severe Acute Respiratory Illness, and asymptomatic high-risk direct contacts of confirmed cases. As on 23 April, 525,667 individuals and 541,789 samples were tested, of which 23,502 samples tested positive.
Even though the number of tests conducted by India has risen from 0.01 per thousand population on 24 March to 0.33/1000 today, it is still far short of the testing done by countries that have been more successful in controlling the virus spread—Hong Kong (17.6/1000), Singapore (16.2/1000), South Korea (11.5/1000), Taiwan 2.5/1000), and Vietnam (2.1/1000), are doing.
Testing per million population in various countries and Kerala as on 23 April 2020
| Country/State | Cases | Deaths | CFR |
Tests per million population |
| India | 23,502 | 722 | 3.1 | 393 |
| Kerala | 447 | 3 | 0.7 | 610 |
| South Korea | 10,708 | 240 | 2.2 | 11,499 |
| Singapore | 11,178 | 12 | 0.1 | 16,203 |
| Hong Kong | 1,036 | 4 | 0.4 | 17,579 |
| Taiwan | 428 | 6 | 1.4 | 2,478 |
| Vietnam | 268 | 0 | 0 | 2,119 |
Aggressive testing detects cases early and prevents further spread of the disease by isolating cases in hospitals or at home. South Korea, Hong Kong and Singapore contained the spread of the virus by testing aggressively and isolating detected COVID-19 cases, a lesson lost on the Indian government,
India is under-testing with the excuse that the COVID-19 outbreak is not yet in Stage 3 community transmission. Kerala tested aggressively and found several cases which otherwise may not have been found. At the time India locked down, Kerala with just two percent of India’s population accounted for 17 percent of the tests conducted. Today the number of tests they have done per thousand population is one and a half times that India has done.
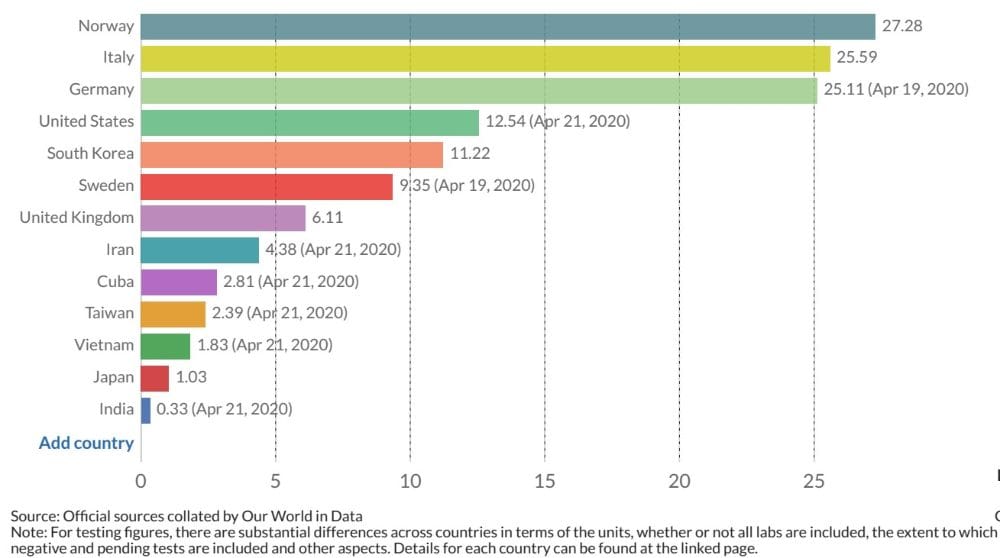
COVID-19 tests conducted per thousand population up to 22 April by selected countries.
A sentinel surveillance study conducted between 15 February and 15 March, by the Indian Council for Medical Research (ICMR) at 51 sites to detect community transmission of COVID-19. None of the samples from 826 persons suffering from severe acute respiratory infection (SARI) or influenza-like illnesses were found to be positive. Another sentinel surveillance study (published on 9 April 2020) done among SARI patients conducted at 41 sites in 20 States/Union Territories from 15 February, found that 1.8 percent of the 5,911 SARI patients tested positive.
[embedded content]
Yet, on 10 April, Lav Agarwal, the Ministry of Health and Family Welfare (MoHFW) spokesperson stated only 320 out of 16,000 samples were positive and that no community transmission had occurred, that is a two percent incidence (though Agarwal claimed it to be 0.2 percent in his interview), which is the about the same incidence the study published on 9 April obtained. The only way to resolve the difference between the results of the ICMR and the other two studies is to ramp up testing.
To ramp up testing, India has decided to import 1 million testing kits and encourage Indian companies to make kits locally. From 5 April, 50 crore persons have become eligible under government’s insurance scheme—Ayushman Bharat for free testing and treatment for COVID-19.
Meagre public health care resources
India has 0.53 public hospital beds per 1,000 population (0.7 beds per 1,000 if private hospitals were included). This compares poorly with China, Iran and Italy that have 4.34, 1.5 and 3.18 hospital beds per 1,000 population. These countries struggled with bed shortage at the peak of the COVID-19 outbreak. South Korea has 13 beds per 1,000 population.
India has a total hospital bed strength of ~10 lakhs beds. A large fraction of this bed strength would be utilized by existing cases. ICU beds constitute 5-7 percent of the total beds, i.e., India has 50,000-70,000 ICU beds. If about half of the ICU beds have ventilators, India would have about 25,000-35,000 ventilators.
India has 0.76 doctors per 1,000 population. These figures do not compare favourably with other countries. China, Iran, and Italy have 1.81, 1.49 and 4.02 doctors per 1,000 population, respectively.
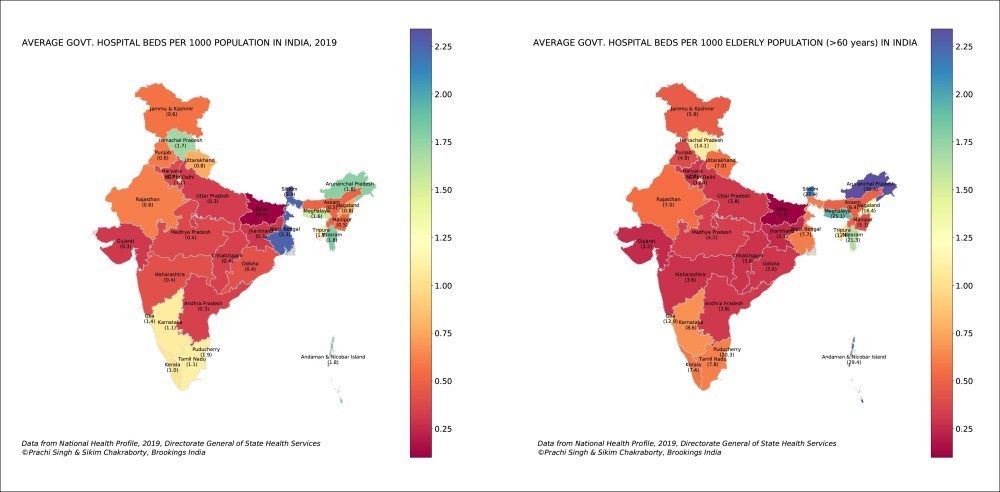
Hospital beds in India per thousand population
India’s public health care system is weak. Efforts are being made to bolster it to meet the COVID-19 challenge. The Indian Railways is converting several railway rakes into mobile hospitals. Other efforts to ramp up bed strength and create dedicated hospitals for COVID-19 will add about 1 lakh beds. India banned the export of ventilators last month and is encouraging Indian industry to make more of them very quickly.
Time will tell whether the additional capacity can carry India through impending future peaks.
Can India’s public health system cope with the impending tsunami of cases?
India’s has had a sharp rise in daily number of cases in the last 3 weeks. The rise may be attributed partially to the ramping up of testing in the last few weeks. The total number of detected cases in India on 23 April is 23,039.
COVID-19 Cases and deaths in India since January 2020 – table
| Dt 2020 | Total confirmed cases | Daily new confirmed cases | Total confirmed deaths |
Daily new confirmed deaths |
| 1 March | 3 | 0 | 0 | 0 |
| 1 April | 1,397 | 146 | 35 | 7 |
| 15 April | 12,370 | 883 | 422 | 29 |
| 23 April | 23,039 | 1,669 | 721 | 40 |
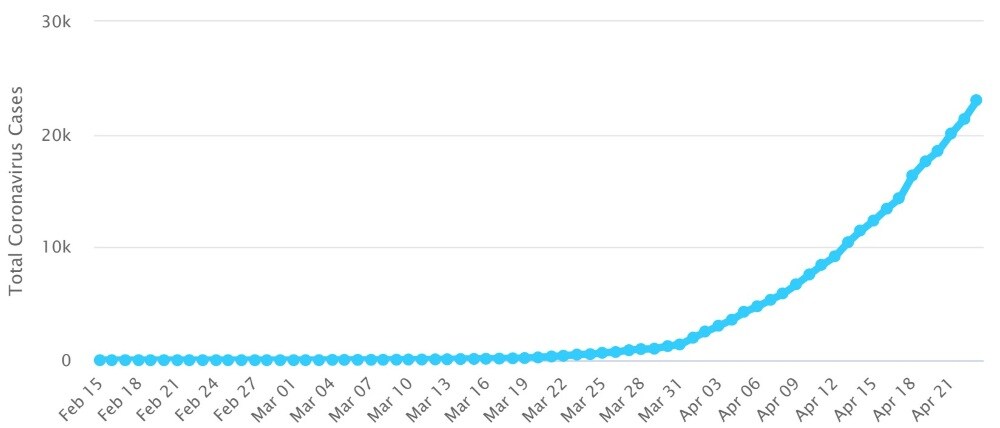
Total detected cases of coronavirus in India.
Case peaking happened in many countries about 30-40 days from the time they first had 30 new cases per day. If India follows the same path, cases may peak towards end-April. However, if India follows the US trajectory, case peaking will happen later and at a higher daily case level.
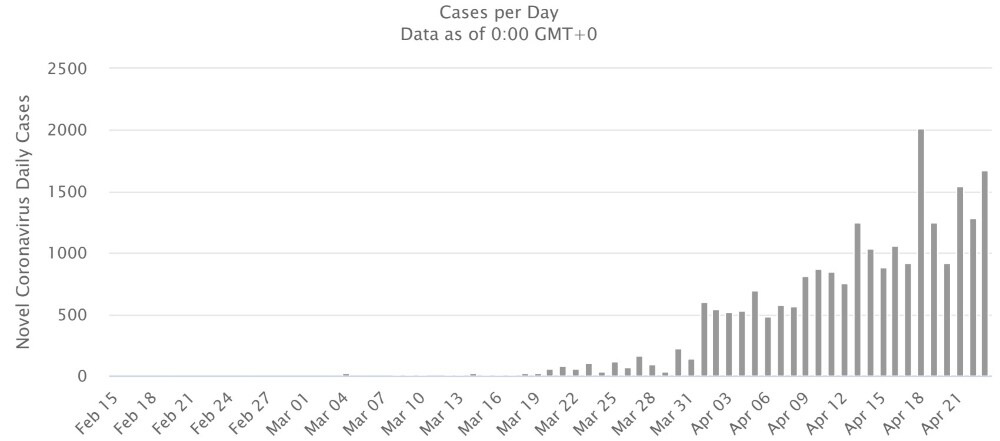
Daily detected new Coronavirus cases in India.
Case incidence with NPI depends on several factors–India’s future control strategy, e.g., number of lockdowns and their periods, efficacy of sanitizing and physical distancing, the strength of the virus strains in India and whether high temperatures reduce its spread. Without knowing India’s control strategy it is difficult to put a figure on how many Indians will be infected before the coronavirus is tamed. Suffice to say that the probability of the peak number of cases that may occur may overwhelm the surge capacity of India’s public health care system is high. If the public health care system is stretched, the rich and the powerful will commandeer a disproportionate share of India’s scarce public health care resources.
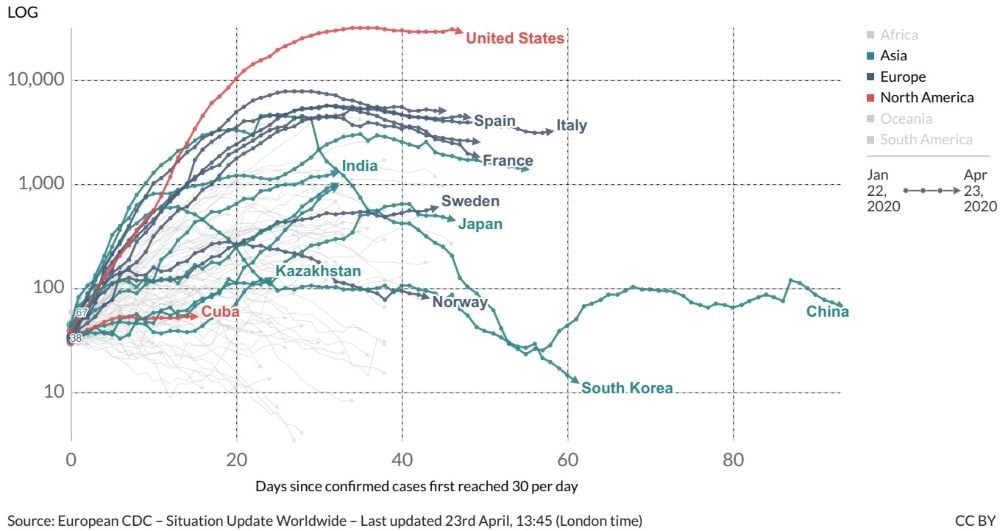
Daily confirmed cases in selected countries
What happens after the lockdown is lifted? Flying blind
Lockdowns provide time to prepare for the next step. They do not solve the problem as they do not remove the virus completely or help develop herd immunity. Until herd immunity happens or a vaccine becomes available, repeated lockdowns may be necessary when case numbers rise alarmingly after lockdowns are lifted. The Imperial College study uses the number of ICU beds being used as on/off trigger numbers for declaring or relaxing lockdowns.
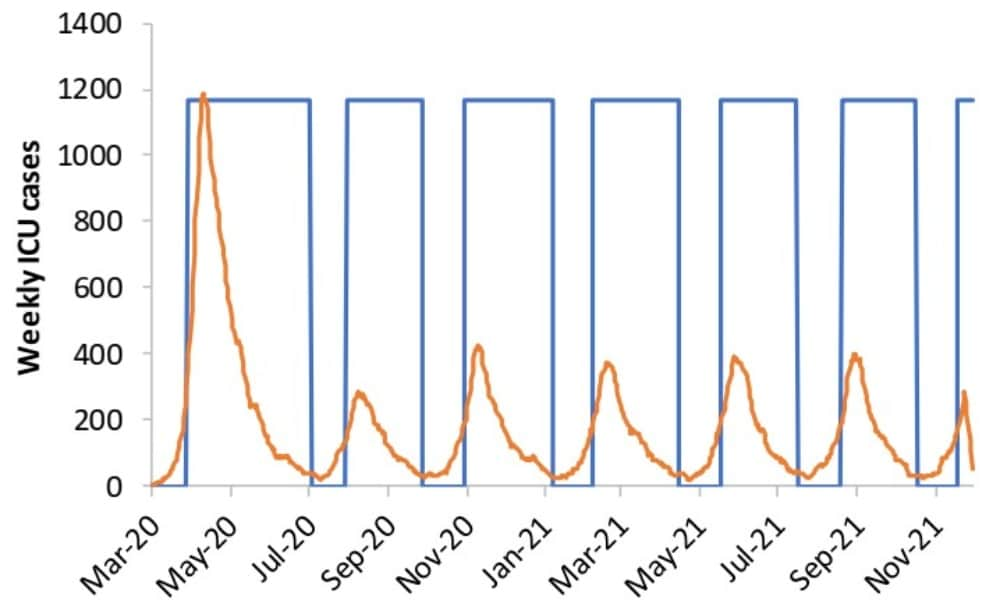
Use of ICU bed requirement as on/off triggers for invoking suppression strategy successively (Imperial College study)
The Singh and Adhikari study also uses case numbers to suggest on/off triggers for locking downs and lifting them.
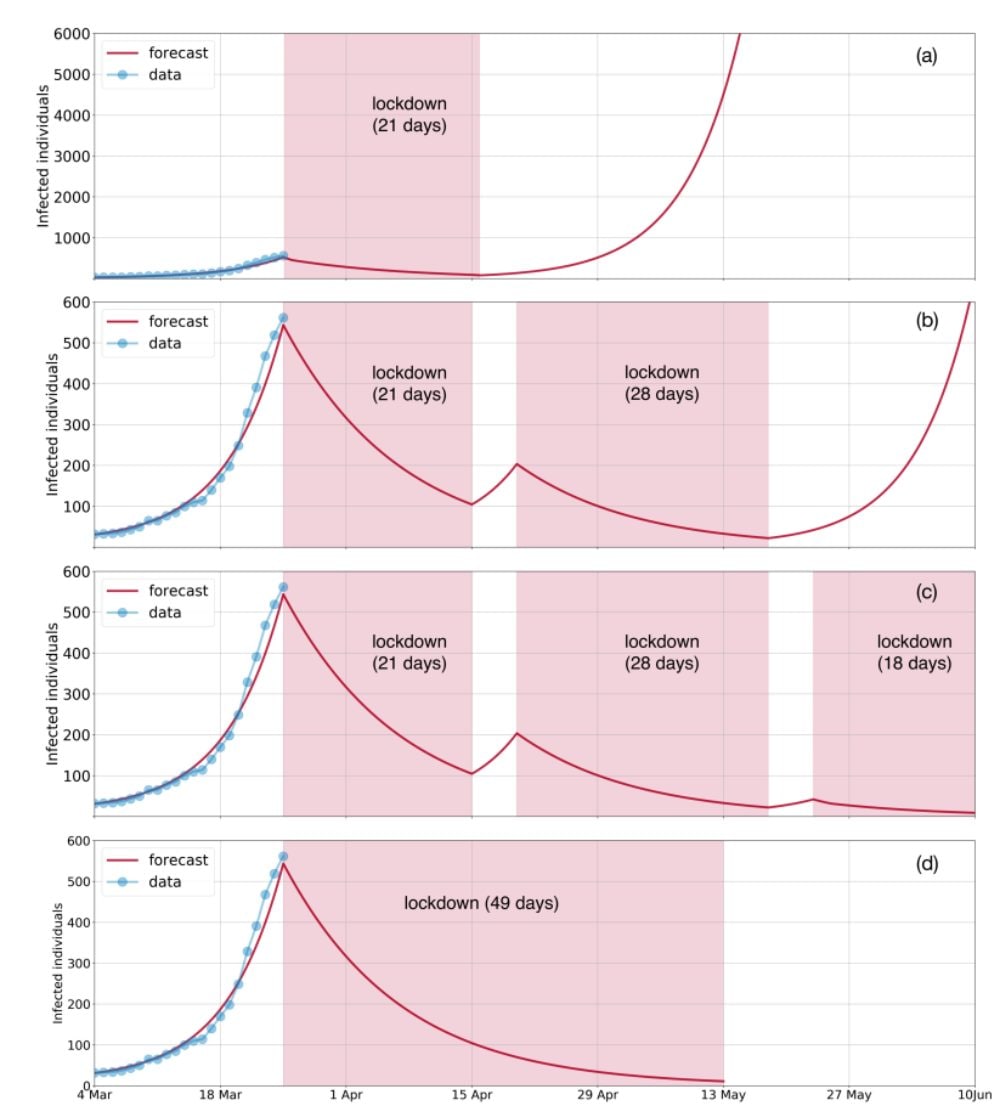
Forecast of cases in India used for lockdown on/off triggers (Singh & Adhikari study)
The government should communicate its strategy to beat the coronavirus and the steps it plans to take after the current lockdown. Else, India will be flying blind.
A sudden shift from mild mitigation to severe suppression strategy: Panic
Why did India suddenly switch from a mild mitigation strategy to a severe suppression strategy without explaining the logic for this action? Case numbers could not have been the reason as there were only 332-396 cases on 22-23 March, around when the lockdown decision may have been taken. An emergency response plan for viral epidemics probably does not exist. None could be located in the public domain, and such documents are not state secrets. A very recently prepared Ministry of Health and Family Welfare document, Containment Plan for Large Outbreaks Novel Coronavirus Disease 2019 (COVID-19) (Containment Plan), does not refer to lockdowns. So existing government plans probably did not influence the lockdown decision.
As risk bearers, the citizens of India have the right to ask their government for an explanation for its actions. Without an explanation from the government for declaring a lockdown, the logical conclusion is that India panicked after the Imperial College study was published and the government realized that it was well prepared for a large outbreak of COVID-19.
Panic is normal in war. It explains why Gen AAK Niazi, the Pakistan army commander in East Pakistan in1971, surrendered to the Indian army even though his troops outnumbered Indian troops by a ratio of 9:1 in Dhaka. But then, Gen JFR Jacob, the Indian army negotiator, did not reveal his troop strength to Gen Niazi, who buckled because of lack of information about the Indian troop strength.
We are at war with the coronavirus. Panic does not win wars; information and preparation do. Sun Tzu, the Chinese general and military strategist who wrote the book The art of war 2,500 years ago was right. In his words, “if you know the enemy,” i.e., in the war against coronavirus, have information about cases–through testing, and how the virus behaves–understanding its transmission dynamics; “and know yourself,” i.e., pre-arm ourself with a good emergency response plan for a viral outbreak, “you need not fear the result of a hundred battles.”
South Korea, Singapore, Taiwan and Hong Kong, frontline countries when the coronavirus war began four months ago, did not panic. They followed Sun Tzu’s advice. They tested to detect infected cases, isolated and treated them, and tracked the disease using hawkeye surveillance methods, and “flattened the curve” much earlier than other countries. There is something to learn from them.
Box 4: Coronavirus timeline for India
Global events
2019
- 2 Dec First known hospitalisation caused by pneumonia with unknown aetiology in Wuhan.
- 12 Dec New viral outbreak first detected in the city of Wuhan.
- 30 Dec Cluster of cases mostly associated with the Seafood market in Wuhan noticed. News of an outbreak of “pneumonia of unknown origin” starts circulating on social media.
- 31 Dec China informs WHO of cases of pneumonia of unknown aetiology detected in Wuhan.
2020
- 8 Jan Chinese scientists announced the discovery of a new coronavirus
- 13 Jan Thailand confirms the first COVID-19 case outside China of a Chinese woman who arrived in Bangkok from China on 8 January.
- 14 Jan Wuhan Health Commission, “We have not found proof for human-to-human transmission. The possibility of limited human-to-human transmission cannot be excluded, but the risk of sustained transmission is low.”
- 14 Jan WHO “Preliminary investigations by the Chinese authorities found no clear evidence of human-to-human transmission of coronavirus.
- 21 Jan Chinese officials acknowledged human-to-human transmission risk. Local outbreaks already seeded in Beijing, Shanghai, other cities.
- 27 Jan WHO declares global health emergency
- 12 Mar WHO declares COVID-29 a pandemic
- 16 Apr World Bank and IMF cancel debts for certain countries
India events
2020
Cases
- 30 Jan First case detected in India–a Thrissur student who had returned from Wuhan University.
- 12 Mar India reports first death.
Travel
- 1 Feb Air evacuation of Indians from Wuhan begins.
- 3 Mar India bans travel from China, Italy, Iran, South Korea.
- 10 Mar Air evacuation of Indians from Iran and Italy begins.
- 12 Mar All visas suspended, barring for diplomats, UN & international body officials, employment & official purposes.
- 19 Mar Some state governments ban public transport.
- 22 Mar All international flights cancelled. All passenger trains cancelled. All non-essential buses cancelled.
- 23 Mar All domestic flights cancelled.
Educational institutions and commercial establishments
- 5 Mar Primary schools start shutting in some states.
- 11 Mar Educational institutions start shutting in some states.
- 12 Mar Cinema halls, malls, pubs ordered shut in some states.
- 17 Mar Important tourist destinations in some states closed.
Social distancing, quarantine, sanitization
- 6 Mar India issues advisory to avoid mass meetings.
- 11 Mar All Indians arriving from COVID-19 hit countries to be quarantined for 14 days.
- 14 Mar Railways remove curtains and blankets from a/c coaches.
- 16 Mar Government issues advisory regarding social distancing.
- 17 Mar Mandatory quarantine of passengers coming from UAE, Qatar, Oman, Kuwait.
Screening, testing, treatment
- 4 Mar Thermal screening of all international arrivals at airports.
- 14 Mar Government names 65 labs for testing.
- 20 Mar Government decides that all pneumonia cases, regardless of travel or contact history are to be tested.
- 21 Mar ICMR issued a notification permitting designated private laboratories to test for Covid-19.
- 5 Apr Testing & treatment to be allowed under Ayushman Bharat insurance scheme will benefit 50 crore people.
Testing kits, medical equipment
- 16 Mar Government made its first bulk order of 10 lakh testing kits.
- 19 Mar Export of mechanical ventilators banned.
- 23 Mar ICMR started approving domestic production of testing kits.
- 24 Mar Export of all respiratory apparatuses and breathing devices banned.
Lockdown
- 22 Mar One day Janata curfew.
- 23 Mar District borders closed in some states
- 25 Mar 3-week countrywide lockdown starts.
- 27 Mar Migrant labour starts mass migration to their villages on foot for lack of transport.
- 29 Mar Some states organize shelter and kitchens for migrant labour.
- 12 Apr Migrant workers riot in Surat demanding transport to go home.
- 14 Apr Lockdown extended till 3 May. Assembly of thousands in Bandra Railway Station because of fake news of trains running.
- 20 Apr Partial lifting of lockdown in some states
Economic package
- 26 Mar Government announces Rs 1.7 lakh crore. 5kg of wheat/rice, 1 kg of pulses to be distributed free to each person every month for ~800 million poor people in the next 3 months; free cooking gas cylinders to 83 million poor families; Rs 500/month to ~200 million poor women for next 3 months; one-time cash transfer of Rs 1,000 to 30 million senior citizens.
Other events
- 13 Mar Prime Minister proposes that South Asian countries fight COVID-19 jointly.
- 14 Mar Union government declares the pandemic as a notified disaster under the Disaster Management Act. National Institute of Virology isolates a strain of the novel coronavirus.
The author is an environmental engineer with specialization in risk analysis
Also Read:
Is the COVID-19 pandemic a black swan or a gray rhino event? — Part 1
Thie COVID-19 pandemic threatens to overwhelm India’s health care system
Updated Date: Apr 25, 2020 13:24:22 IST
Tags : Coronavirus, Coronavirus Outbreak, Death Rate Of Coronavirus, Economy, Effects Of Pandemic, Icu Beds, Lockdown, Pandemic, Spread Of Coronavirus, Testing, Treatment, Virus, WHO
Post a Comment